- गोवा सरकारGovernment Of Goa
- स्वास्थ्य एवं परिवार कल्याण मंत्रालय

Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana
Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana, the flagship scheme of Hon’ble Prime Minister of India was launched in the State of Goa on 23rd September 2018, along with National launch.
The objective of AB-PMJAY to reduce catastrophic health expenditure, improve access to quality health care, reduce unmet needs and reduce out of pocket healthcare expenditures of poor and vulnerable families of the Socio-Economic Caste Census (SECC) database of the State. These eligible AB-PMJAY beneficiary families will be provided coverage for secondary, tertiary and day care procedures for treatment of diseases and medical conditions through a network of Empanelled Health Care Providers (EHCP).
PMJAY provides health cover of up to Rs. 5, 00,000 per family per year. No restrictions on family size, age or gender.PM-JAY has defined around 1,652 medical packages in Goa for covering surgery, medical and day care treatments.
A total of 36,431 families are Eligible for AB-PMJAY in the State of Goa. 28,219 individuals are registered under AB-PMJAY as on 31/05/2023 and in that registered identified families are around 10,254.
PM-JAY provides cashless cover of up to INR5,00,000 to each eligible family per annum for listed secondary and tertiary care conditions. The cover under the scheme includes all expenses incurred on the following components of the treatment.
- Medical examination, treatment and consultation
- Pre-hospitalization
- Medicine and medical consumables
- Non-intensive and intensive care services
- Diagnostic and laboratory investigations
- Medical implantation services (where necessary)
- Accommodation benefits
- Food services
- Complications arising during treatment
- Post-hospitalization follow-up care up to 15 days
The benefits of INR 5,00,000 are on a family floater basis which means that it can be used by one or all members of the family. The RSBY had a family cap of five members. However, based on learnings from those schemes, PM-JAY has been designed in such a way that there is no cap on family size or age of members. In addition, pre-existing diseases are covered from the very first day. This means that any eligible person suffering from any medical condition before being covered by PM-JAY will now be able to get treatment for all those medical conditions as well under this scheme right from the day they are enrolled.
Coverage under PM-JAY
Including the poorest and most vulnerable population of any country in the health insurance programme is often the most challenging because they cannot pay any premium and are the hardest to reach. Many times they are also not literate and, therefore, require a very different approach for awareness generation. This is true for most Lower and Middle-Income Countries (LMIC) and India is not an exception.
Thus, PM-JAY has been rolled out for the bottom 40 per cent of poor and vulnerable population. In absolute numbers, this is close to 10.74 crore (100.74 million) households. The inclusion of households is based on the deprivation and occupational criteria of the Socio-Economic Caste Census 2011 (SECC 2011) for rural and urban areas, respectively. This number also includes families that were covered in the RSBY but were not present in the SECC 2011 database.
The SECC involves ranking of the households based on their socio-economic status. It uses exclusion and inclusion criteria and accordingly decides on the automatically included and automatically excluded households. Rural households which are included (not excluded) are then ranked based on their status of seven deprivation criteria (D1 to D7). Urban households are categorised based on occupation categories.
In line with the approach of the Government to use the SECC database for social welfare schemes, PM-JAY also identifies targeted beneficiary families through this data.
Rural Beneficiaries
Out of the total seven deprivation criteria for rural areas, PM-JAY covered all such families who fall into at least one of the following six deprivation criteria (D1 to D5 and D7) and automatic inclusion(Destitute/ living on alms, manual scavenger households, primitive tribal group, legally released bonded labour) criteria:
- D1- Only one room with kucha walls and kucha roof
- D2- No adult member between ages 16 to 59
- D3- Households with no adult male member between ages 16 to 59
- D4- Disabled member and no able-bodied adult member
- D5- SC/ST households
- D7- Landless households deriving a major part of their income from manual casual labour
Urban Beneficiaries
For urban areas, the following 11 occupational categories of workers are eligible for the scheme:
- Ragpicker
- Beggar
- Domestic worker
- Street vendor/ Cobbler/hawker / other service provider working on streets
- Construction worker/ Plumber/ Mason/ Labour/ Painter/ Welder/ Security guard/ Coolie and other head-load worker
- Sweeper/ Sanitation worker/ Mali
- Home-based worker/ Artisan/ Handicrafts worker/ Tailor
- Transport worker/ Driver/ Conductor/ Helper to drivers and conductors/ Cart puller/ Rickshaw puller
- Shop worker/ Assistant/ Peon in small establishment/ Helper/Delivery assistant / Attendant/ Waiter
- Electrician/ Mechanic/ Assembler/ Repair worker
- Washer-man/ Chowkidar
Even though PM-JAY uses the SECC as the basis of eligibility of households, many States are already implementing their own health insurance schemes with a set of beneficiaries already identified. Thus, States have been provided the flexibility to use their own database for PM-JAY. However, they will need to ensure that all the families eligible based on the SECC database are also covered.
Expansion of coverage by States under PM-JAY and convergence
Various States have been implementing their own health insurance/assurance schemes over the past couple of decades. Most of these schemes provide cover for tertiary care conditions only. The benefit cover of these schemes is mostly available within the State boundaries except some smaller States have empanelled a few hospitals outside the State boundaries. Very few States had converged their schemes with the erstwhile RSBY scheme and many of them were operating independently. This was due to the lack of flexibility in the design of the RSBY, which although initially helped in quick scale-up but became a challenge over a period of time and offered limited flexibility to the States.
Even though these schemes were targeting the poor and vulnerable, there were large variations across States in terms of eligibility criteria and databases. Few States were using the food subsidy database while some others had created a separate database for their welfare schemes.
The primary objectives for launching PM-JAY were to ensure comprehensive coverage for catastrophic illnesses, reduce catastrophic out-of-pocket expenditure, improve access to hospitalisation care, reduce unmet needs, and to converge various health insurance schemes across the States. PM-JAY will also establish national standards for a health assurance system and is providing national portability of care. At the implementation level, the States are given the flexibility to use their own database if they were already implementing a health insurance/ assurance scheme and were covering more families than those eligible as per the SECC 2011 database. However, such States shall ensure that all families eligible as per the SECC data are covered and not denied benefits.
| Sr No. | Name of Staff | Designation |
| 1 | Dikshita D. Borkar | Operations Manager |
| 2 | Siddesh Gawas | Finance Manager |
| 3 | Pooja Naik | Monitoring & Evaluation Manager |
| 4 | Ruben D’Costa | IT Support cum Data Manager |
| 5 | Krupali L. Majik | Accounts Assistant |
 -Social Media (Official DHS Facebook handle)
-Social Media (Official DHS Facebook handle)
 -Felicitated all PHCs on identifying beneficiaries & creating golden card records
-Printing of face masks for beneficiaries.
-Felicitated all PHCs on identifying beneficiaries & creating golden card records
-Printing of face masks for beneficiaries.Frequently Asked Questions on Ayushman Bharat Pradhan Mantri – Jan Arogya Yojana (AB PM-JAY)
=
What is Ayushman Bharat Pradhan Mantri Jan Arogya Yojana?
In Goa, Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) is a Health Assurance Scheme for citizens – especially the poor and vulnerable groups as per the latest Socio-Economic Caste Census (SECC) data of 2011.
What benefits are available under AB PM-JAY?
AB PM-JAY provides a health assurance cover upto Rs 5 lakh per family, per year for secondary and tertiary hospitalization.
All pre-existing conditions are covered under AB PM-JAY.
What health services are available under AB PM-JAY?
Entire Hospitalization expenses, day care surgeries, follow-up care, pre and post hospitalization expense benefits and new born child/children services. The comprehensive list of services is available on https://www.pmjay.gov.in
Who is eligible to avail benefits under AB PM-JAY?
There are 36,431 families eligible in Goa under AB PM-JAY.
These beneficiaries are identified as deprived rural families and occupational categories of urban workers’ families as per the latest SECC data.
Will beneficiaries have to pay anything to get covered under this scheme?
No. AB PM-JAY is a cashless and paperless health services. All eligible beneficiaries can avail free services for secondary and tertiary hospital care for identified packages at public hospitals and empanelled private hospitals.
What is the enrolment process? Is there any time period for enrolment?
ABPM-JAY is an entitlement-based mission. There is no enrolment process. Families who are identified by the government on the basis of deprivation and occupational criteria using the SECC database both in rural and urban areas are entitled for AB PM-JAY.
There is no time frame; beneficiaries can get their E-Cards generated any time prior to hospitalization.
Families whose names are not present in SECC data, can avail the benefits under AB PM-JAY?
No new families can be added under AB PM-JAY. However, names of additional family members can be added by submitting Birth Certificate/Marriage certificate for existing SECC Families.
Will a card be given to the beneficiary?
A dedicated AB PM-JAY family identification number will be allotted to eligible families. Additionally, an e-card will also be given to the beneficiary at the time of hospitalization.
If I am listed as a beneficiary and I need to be hospitalized, what documents do I need to bring to the hospital?
At the time of admission to the hospital, beneficiaries should carry ration cards or any other government recognized photo identity document like Aadhaar etc.
What happens if I fall ill during my travel or when I am out of my district or state?
The scheme has a portability feature wherein beneficiaries can avail services across all the implementing States/UTs.
Can my brother/sister who is married be eligible under AB PMJAY?
No, they are not eligible for the same.
Where can I find the list of empanelled hospitals under AB PMJAY?
On the AB PMJAY website, the link is https://hospitals.pmjay.gov.in/Search/
The List of Empanelled hospitals as on 25th May 2023 under AB PMJAY are: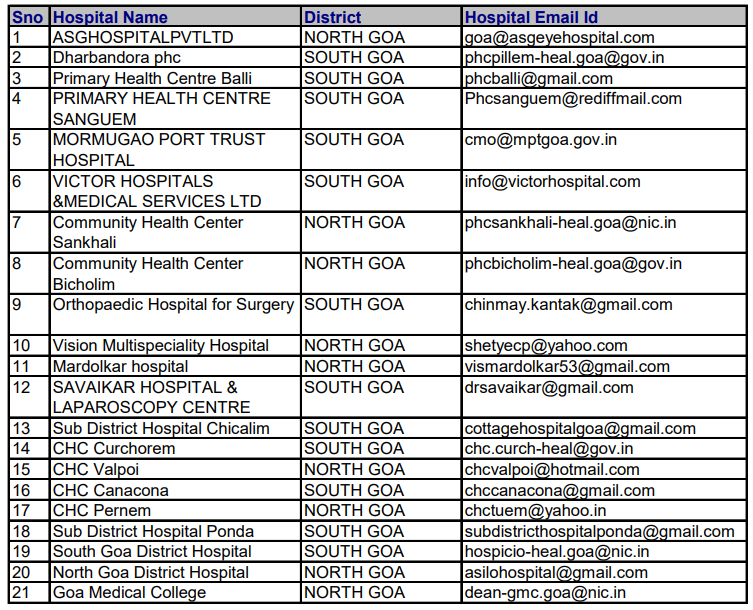
Is pregnancy covered under AB PM-JAY?
Yes.
Are Already existing illnesses covered under this scheme?
Yes.
Are Benefits available for a new born child under this scheme?
Yes.
Is there any capping on the age of family members?
No, there is no capping on the age of family members, any age group are eligible for this scheme.
What is the helpline number for AB PM-JAY?
The patient may contact the toll-free helpline number 14555 for support or reach out to Ayushman Mitra in the hospital.
Benefits under this scheme can be available without an Aadhar Card?
Aadhaar is not mandatory to avail benefits for the first time.
However, Aadhaar is compulsory for those seeking treatment for the second time.
How can families be added in the list to avail benefits under AB PM-JAY?
No new families can be added under PM-JAY.
However, names of additional family members can be added for those families whose names are already on the SECC list.
What documents do I require under Ayushman Bharat Pradhan Mantri Jan- Arogya Yojana (ABPM-JAY)?
The following documents will be required during the application process.
- A certified document confirming your age and identification.
- Existing contact details of the buyer
- Income certificate
- Cast certificate
- A document stating the current family status.
Can my wife be added as i am already a AB PMJAY Beneficiary? (Documents Needed)
Yes, she can be added. Documents required: Ration Card / Marriage certificate.
Does the AB PM-JAY cover natural death, suicide or death due to some illness/ disease/ pregnancy?
No, AB PM-JAY is not a life insurance scheme it is a Health Insurance Scheme.
How can I link my Mobile Number with AB PMJAY?
You can link your mobile no at the time of BIS enrolment. However, as of now there is no option of updating your mobile no once the e-card is generated.
How can I know I am eligible for AB PMJAY Scheme?
To find your eligibility you can visit https://mera.pmjay.gov.in/search/login or
Can visit the nearest empanelled hospital under AB PMJAY
In case of problems faced by AB PMJAY Beneficiaries whom can they contact?
The State Health Agency (SHA), Directorate of Health Services, Campal – Goa.
State Health Agency
Ayushman Bharat Pradhan Mantri Jan Arogya Yojana
Address: Directorate of Health Services, Campal, Panaji, Goa
Contact No. 0832-2225668
Email Id: pmjaygoa[at]gmail[dot]com
National Toll-Free Call Center Number: 14555
Subscribe to our
Newsletter
***We Promise, no spam!